The Trauma and Addiction Connection
 Addiction science has come a long way in recognizing the undercurrents of substance use disorder (SUD) and alcohol use disorder (AUD). A primary pivotal point is an understanding that people sometimes take drastic measures to alleviate their pain, even if it means compromising their health in other ways.
Addiction science has come a long way in recognizing the undercurrents of substance use disorder (SUD) and alcohol use disorder (AUD). A primary pivotal point is an understanding that people sometimes take drastic measures to alleviate their pain, even if it means compromising their health in other ways.
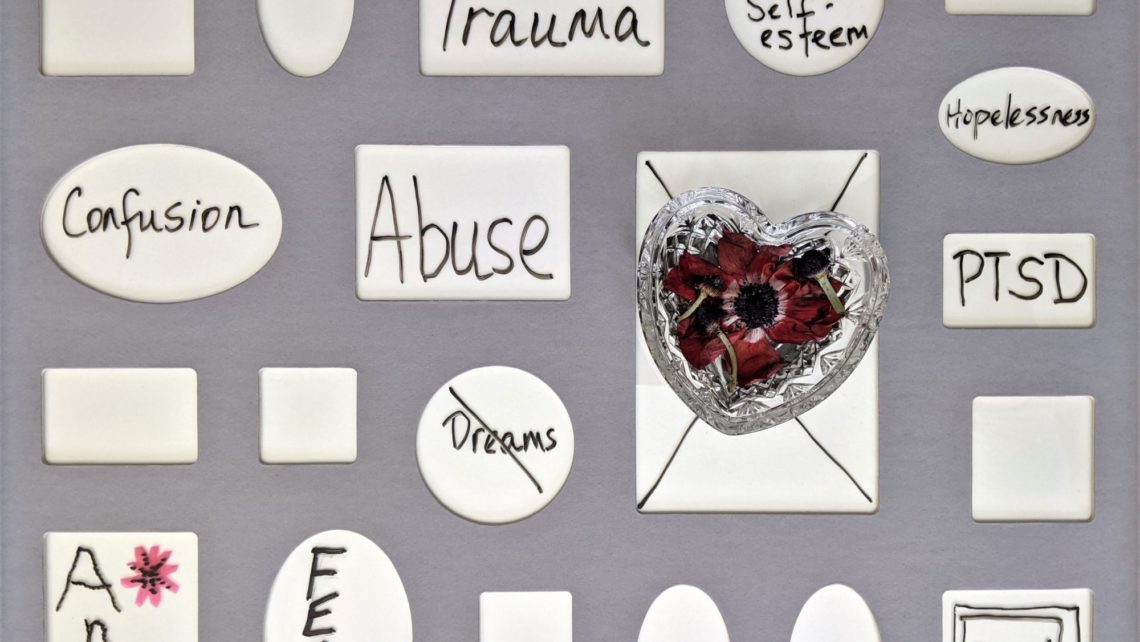
The Impact of Trauma
What is trauma? The clinical definition, according to the Trauma-Informed Care Implementation Resource Center (TICIRC) is, “Trauma is a pervasive problem. It results from exposure to an incident or series of events that are emotionally disturbing or life-threatening with lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, and/or spiritual well-being.”
Traumatic experiences children and adults might suffer include, but aren’t limited to:
- Abrupt, unexplained separation from or loss of a loved one
- Bullying, discrimination, oppression, and racism
- Childhood neglect
- Emotional, physical, and sexual abuse
- Homelessness or poverty
- Living with a family member with mental health disorders, SUD, AUD, or who has attempted or died by suicide
- Violence in the community, terrorism, or war
TICIRC indicates that anyone of any age, cultural background, or financial status can suffer trauma. However, adults who had four or more adverse childhood experiences (ACEs) like the ones described above are:
- “7 times more likely to consider themselves alcoholics.”
- “10 times more likely to have injected street drugs.”
- “12 times as likely to have attempted suicide.”
Why does this happen?
Just Trying to Cope
The National Institute on Drug Abuse (NIDA) states that triggers are often the catalyst for people with traumatic experiences to turn to drugs or alcohol. Known as “maladaptive behavior,” choosing substances numbs the pain more quickly and allows the person to ignore the stressor, memory, or situation. Consider the following rationale regarding contributing triggers/stressors from NIDA:
- “Trouble at home. If your home is an unhappy place, or was when you were growing up, you might be more likely to have a drug problem. When kids aren’t well cared for, or there are lots of fights, or a parent is using drugs, the chance of addiction goes up.”
- “Mental health problems. People who have untreated mental health problems, such as depression or anxiety, or untreated attention-deficit/hyperactivity disorder (ADHD) are more likely to become addicted. They might use drugs to try to feel better.”
- “Trouble in school, trouble at work, trouble with making friends. Failures at school or work, or trouble getting along with people, can make life hard. You might use drugs to get your mind off these problems.”
Additionally, TICIRC states that “these coping mechanisms may provide some relief, but they can also simultaneously contribute to anxiety, social isolation, and chronic diseases.”
Trauma and addiction are opposing trains on the same track. Tragically, since addiction is a brain disease, this means that most people develop a dangerous chemical dependency as well as trying to deal with the complications of their underlying trauma.
Acknowledging Trauma to Start the Healing Process
Recognizing and moving through traumatic experiences is more than just sitting down with a mental health professional, although that’s a fine starting point.
TICIRC outlines a few other methods that should be part of a comprehensive recovery plan:
- “Protective factors, such as supportive relationships with family members, a teacher, or others in the community, can help shield individuals from the effects of trauma and build resilience to help overcome adversity and confront challenges.”
- “Trauma-informed approaches to care, including relational healing and trauma-specific treatments, can help patients begin processing their experiences in a healthy way.”
At Seabrook, another component in trauma recovery programming includes proven holistic therapies such as:
Eye movement desensitization and reprocessing, or EMDR. This integrative psychotherapy approach has helped relieve psychological distress for millions of clients from all walks of life. As a mental health intervention tool, EMDR has undergone exhaustive research to prove its efficacy for helping people overcome their trauma and live normal, healthy, and well-adjusted lives.
Brainspotting therapy. This relatively recent innovation has a promising future as a therapy for victims of trauma, especially for PTSD. Brainspotting therapy is of special interest in the mental health profession due to the unique way this treatment activates specific areas of the brain. As researchers now know, when individuals with PTSD discuss their traumatic experience, the part of the brain responsible for vision activates. During a brainspotting session, a therapist helps clients position their eyes in ways that stimulate specific regions of the brain, which can lead to healing from trauma.
Turn to Seabrook for Quality Care
We all experience trauma differently, and it’s not something that automatically goes away just because we want it to. There’s value to addressing this conflict directly with qualified professionals who won’t leave you alone on your journey toward a healthier well-being.
The most important factor in trauma and addiction recovery is for a person to receive individualized treatment tailored to their specific emotional and medical needs. At Seabrook, our team of experts work together to provide you with a spectrum of thorough solutions. Resolve your past so you can create a better future. Call us today to learn how we can help.
For further reading: ISTSS: “Traumatic Stress and Substance Abuse Problems”